Hyperactive Neural Networks - Exploring Epilepsy
My best friend, Ella, was diagnosed with epilepsy at the age of 7.
From biking to school, swimming, travelling on public transport, or even staying overnight at a friend’s house for a sleepover, Ella had to be more cautious compared to most of the other kids at school. For her safety, she had to avoid doing these activities on her own, which reduced her independence. Before learning about her condition, I used to take a lot of these day-to-day activities for granted.
You may be wondering why learning about epilepsy should matter to you, especially if you do not have the condition yourself. However, epilepsy affects around 50 million people globally, so it is likely that you could have a loved one, a friend, or even an acquaintance during your lifetime who is affected by epilepsy.
Years of stereotypes, stigma, and superstition have had a negative impact on people living with epilepsy. Examples range from social isolation to prejudice in employment prospects or access to healthcare resources. Many people still incorrectly believe that epilepsy is incurable or even contagious. Another false belief is that people with epilepsy are not as smart as neurotypical people - however, epilepsy does not affect thinking and decision-making except for the duration of a seizure.
Therefore, if someone you know or love has epilepsy, learning about the condition is the first step towards reducing any false misconceptions that you may have. Instead of being afraid of them, pitying them, or being indifferent to their condition, we need to change our mindset to a proactive one.
Looking back to my childhood memories, one of the most important lessons that I learnt was that I should not have been afraid to ask Ella more questions about her condition. I often felt that asking too many questions would be considered rude, and would have been like overstepping a boundary on my part.
However, over time, I realised that it is usually acceptable and often encouraged to be curious, provided that your questions are considerate. As long as your friend or loved one is willing to answer questions about their medical condition and does not feel upset by them, being proactive as opposed to indifferent could help them feel more understood and help you become more supportive with your words and actions.
Alongside the psychosocial aspects of epilepsy, there are also biological factors that need to be considered in order to understand the causes, symptoms, and treatments for epilepsy. Epilepsy is characterised by recurring, involuntary seizures. An epileptic seizure is caused when the brain experiences sudden bursts of electrical activity which impact how neurons or nerve cells communicate with each other. As a result, involuntary movements of the body, loss of consciousness, and sudden changes in one’s emotions are common symptoms during an epileptic fit.
A common myth is that anyone who has had a seizure before must be an epileptic patient. However, a seizure is not always related to epilepsy - in fact, it can occur to anyone. A hiccup is a common example of a brief and usually harmless seizure and it is known as a myoclonus, a type of muscle jerk that one cannot control. If you have ever had a sleep start, a muscle contraction which wakes you up right as you were about to fall asleep, you’ve experienced a brief myoclonus.
While anyone can experience a seizure, people with epilepsy have a lower seizure threshold which means that they are more likely to experience seizures of higher intensity and frequency. Epileptic seizures are generally caused by a genetic risk factor or brain injury which leads to abnormal neural activity.
Non-epileptic seizures, on the other hand, can be caused by environmental triggers like one’s diet, certain medications, and even flashing lights or images. These seizures occur in non-epileptic brain tissue, so there is usually no disruption to the brain’s neural activity. It is essential to be able to distinguish between epileptic and non-epileptic seizures, the reason being that anti-epileptic drugs cannot effectively treat non-epileptic seizures.
When my friend, Ella, was first diagnosed with epilepsy, she started with mild and virtually unnoticeable seizures. These seizures can be detected using technological equipment such as an electroencephalogram (EEG), which records the location of brain activity in an epileptic patient and helps classify seizures. The two main types of seizures which can be classified using an EEG are focal onset seizures and generalised onset seizures.
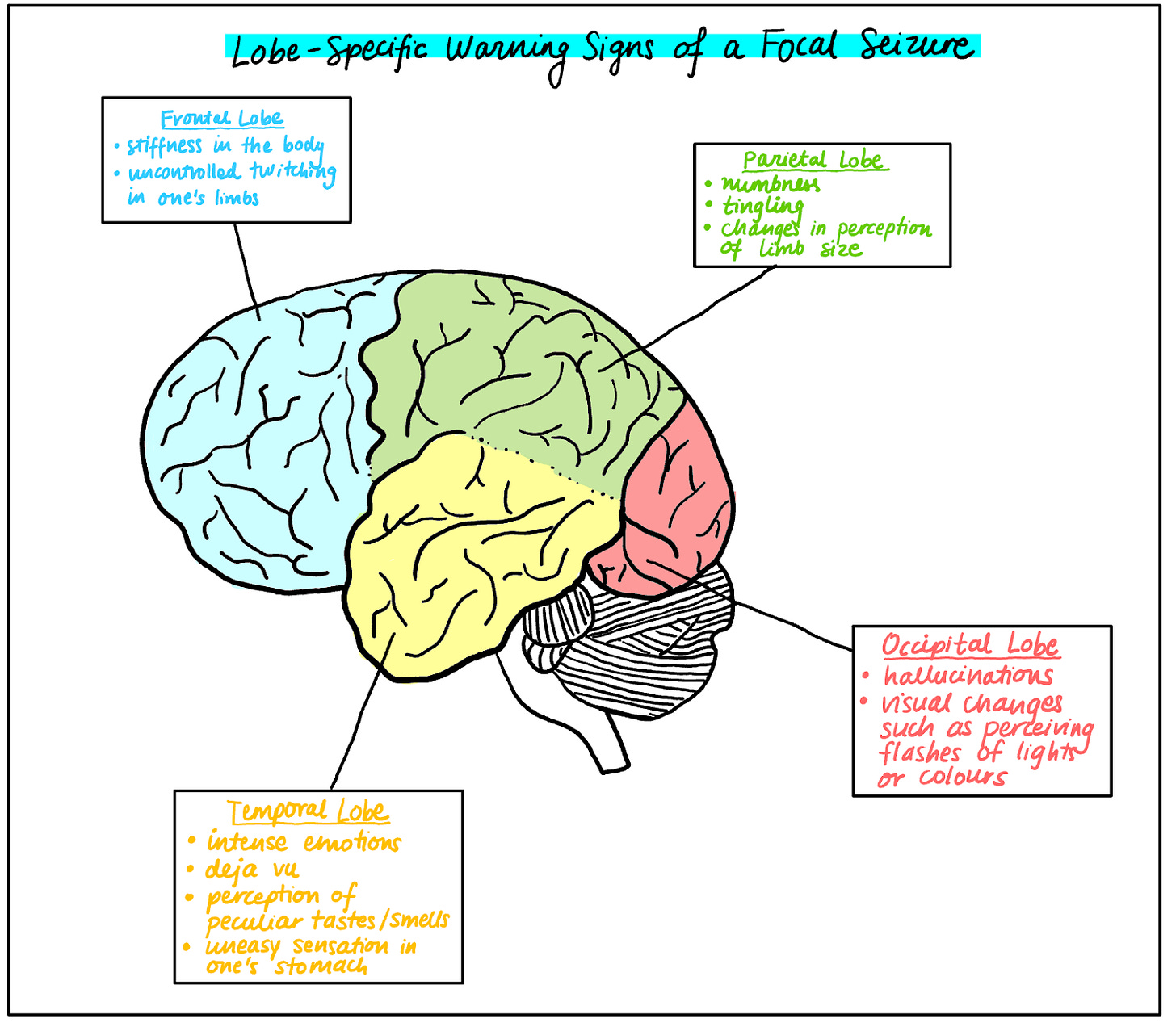
Focal onset seizures start in a specific region or lobe of the brain but may spread to other areas as well. Some epileptic patients retain awareness during a seizure but others may feel disorientated or even become unconscious. Depending on the lobe in which the seizure starts, the warning signs of a focal seizure can be very different and can range from changes in one’s visual perception to intense emotions like fear or anxiety (see figure 1).
Figure 1: A rough illustration of the brain and examples of warning signs for a focal seizure - these signs can change depending on the lobe where the seizure has originated.
Generalised onset seizures involve various regions of the brain and may therefore leave a more negative impact on the patient. For instance, tonic seizures refer to a prolonged tension of one’s muscles which involve most parts of the brain and therefore affect both sides of the body. Atonic seizures, on the other hand, refer to muscles becoming weakened. This often means that a patient experiencing either a tonic or an atonic seizure could fall down if they were originally standing and potentially injure themselves.
In Ella’s early childhood, she experienced absence seizures, which fall under the category of generalised onset seizures. Absence seizures often start in childhood and can cause one to suddenly lose awareness and stop what they are currently doing. This is often accompanied by involuntary muscle jerks or eyelid movements. People may not even notice that a child is experiencing an absence seizure and could instead mistake this brief loss of awareness for daydreaming.
Epilepsy occurs when signalling between neurons or nerve cells goes awry in the brain. Therefore, in order to understand the cause of epilepsy, it is first essential to understand how healthy neural signalling works.
Neurons are specialised nerve cells that help pass electrical impulses throughout the body to respond to different stimuli. Healthy signalling between neurons is necessary for the brain to carry out normal cognitive functions.
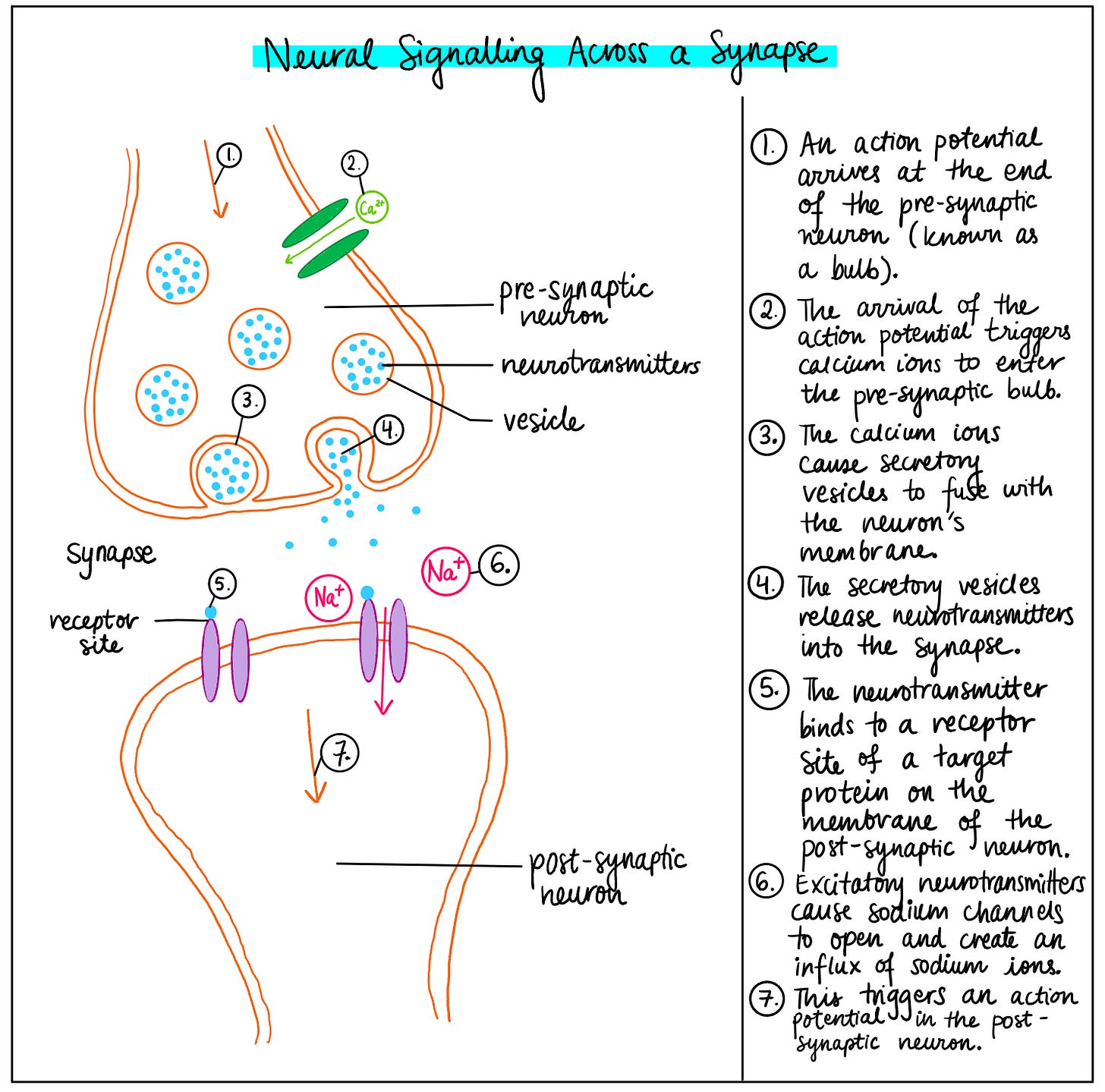
The space between any two neurons is known as a synapse, and electrical impulses cannot pass through this synaptic gap. Instead, when an electrical impulse or an action potential arrives at a pre-synaptic neuron, an inward influx of calcium ions into the pre-synaptic neuron causes sacs called vesicles in this neuron to release neurotransmitters. Neurotransmitters are substances that diffuse out into the synaptic gap and bind to receptor proteins on the post-synaptic neuron (see figure 2).
If the neurotransmitter is excitatory, sodium gated ion channels open and allow positive sodium ions to rush into the post-synaptic neuron. This causes depolarisation or a less negative charge inside the neuron, allowing for the triggering of the next action potential. In this manner, electrical signals are passed along from neuron to neuron.
If the neurotransmitter is inhibitory, chloride gated ion channels open and allow negative chloride ions to rush into the post-synaptic neurons, which causes hyperpolarisation or a more negative charge inside the cell. This reduces the likelihood of the neuron firing and prevents an electrical impulse from being transmitted.
Figure 2: An annotated diagram exploring the process of healthy signalling or communication between neurons, across the synaptic gap.
So, how does neural signalling differ in the brain of an epileptic patient like Ella? Well, communication between neurons changes depending on whether the signals being transmitted are excitatory or inhibitory signals. Glutamate, for example, is an excitatory neurotransmitter which increases the likelihood of a neuron firing. On the other hand, gamma-aminobutyric acid (GABA) is an inhibitory neurotransmitter which reduces the likelihood of a neuron firing. Risks like genetic factors can lead to a disruption in the balance between these signals. Epileptic seizures are caused when there is a high amount of excitatory signalling and low amounts of inhibitory signalling which can cause multiple neurons to fire simultaneously.
Increased sprouting of excitatory axons from existing neurons can lead to greater connectivity between neurons, which also increases the likelihood of more excitatory networks in the brain. Changes in gene expression and genetic mutations can strengthen sodium ion channels or weaken chloride ion channels, which also leads to increased excitatory signalling. Additionally, inhibitory neurons can sometimes be pruned or removed from the brain which can also cause abnormal amounts of excitation in the brain, leading to involuntary muscle contractions or a loss of awareness.
Some of the most common methods used to help reduce the intensity of epileptic seizures include anti-epileptic drugs (AEDs). A range of approved AEDs such as carbamazepine, phenytoin, and benzodiazepines are used to help regulate seizures. AEDs like carbamazepine and phenytoin can inactivate sodium channels, preventing large sodium influxes into neurons and reducing the excitatory signals associated with epilepsy. Benzodiazepines can bind to GABA receptors and help improve the effectiveness of GABA’s inhibitory signalling, reducing the likelihood of neurons firing. AEDs can therefore control levels of excitation and inhibition within neural pathways, helping regulate seizures.
During Ella’s journey with epilepsy, doctors prescribed various AEDs to try and stop her seizures. However, each time she took a new medication, her seizures actually worsened. Removing the previous medication and taking a new one did not help her at all. In fact, she was prescribed 8 different pharmaceutical drugs, and none helped put an end to the seizures. Ella’s case is a real-life example illustrating how traditional medicine such as AEDs may not always work on each and every individual.
Drug-induced aggravation of epilepsy is actually a common clinical problem - for instance, taking carbamazepine can sometimes worsen absence seizures as well as atonic seizures. Furthermore, chemical reactions between various drugs, existing medical conditions, and sudden withdrawal of a medication can also cause serious health problems for a patient with epilepsy, so it is essential to make an accurate diagnosis to avoid prescribing an ineffective or harmful drug.
If AEDs do not prove to be effective and a patient’s seizures begin to considerably harm their general health and safety, surgical intervention may become necessary. Resection surgeries, for instance, involve removing regions of brain tissue that have been causing the seizures. In extremely severe cases, the corpus callosum, a bundle of nerve fibres which connects the two hemispheres of the brain, is cut in order to prevent seizures from affecting both sides of the brain and reducing injuries from seizure-related falls. While other parts of the brain can often take over the functions of the removed tissue, considerable impairment to cognitive functions like communication or decision-making can occur as a result of surgical intervention - this is why surgery is only used as a last resort.
In Ella’s case, traditional medication had not been effective. After some time, her family made a tough decision to transition to alternative medicine such as Ayurveda, Chinese medicine, and CBD. The use of alternative medicine is not usually recommended in medical papers, since it often lacks rigorous testing using double-blind trials. Additionally, alternative medicine is often believed to only have a placebo effect or a psychologically-based improvement in one’s medical condition as opposed to a physiological one, since dosages differ between products and there is often insufficient data on the effectiveness of these dosages. However, carrying out more clinical trials with specific dosages of alternative medicine and using these to complement rather than replace traditional medicine could help tailor treatments towards individuals for whom traditional medicine does not work.
Ella’s epileptic seizures were brought to an end after a combination of alternative medication and female hormonal changes that occurred during puberty. Gender and age can therefore have a massive impact on the severity of an epileptic patient’s seizures. For instance, during puberty, the increase in female sex hormones like oestrogen and progesterone can slow down or speed up brain activity. This can lead to a change in the intensity of seizures. For Ella, hormonal changes during puberty contributed to the end of her epileptic seizures.
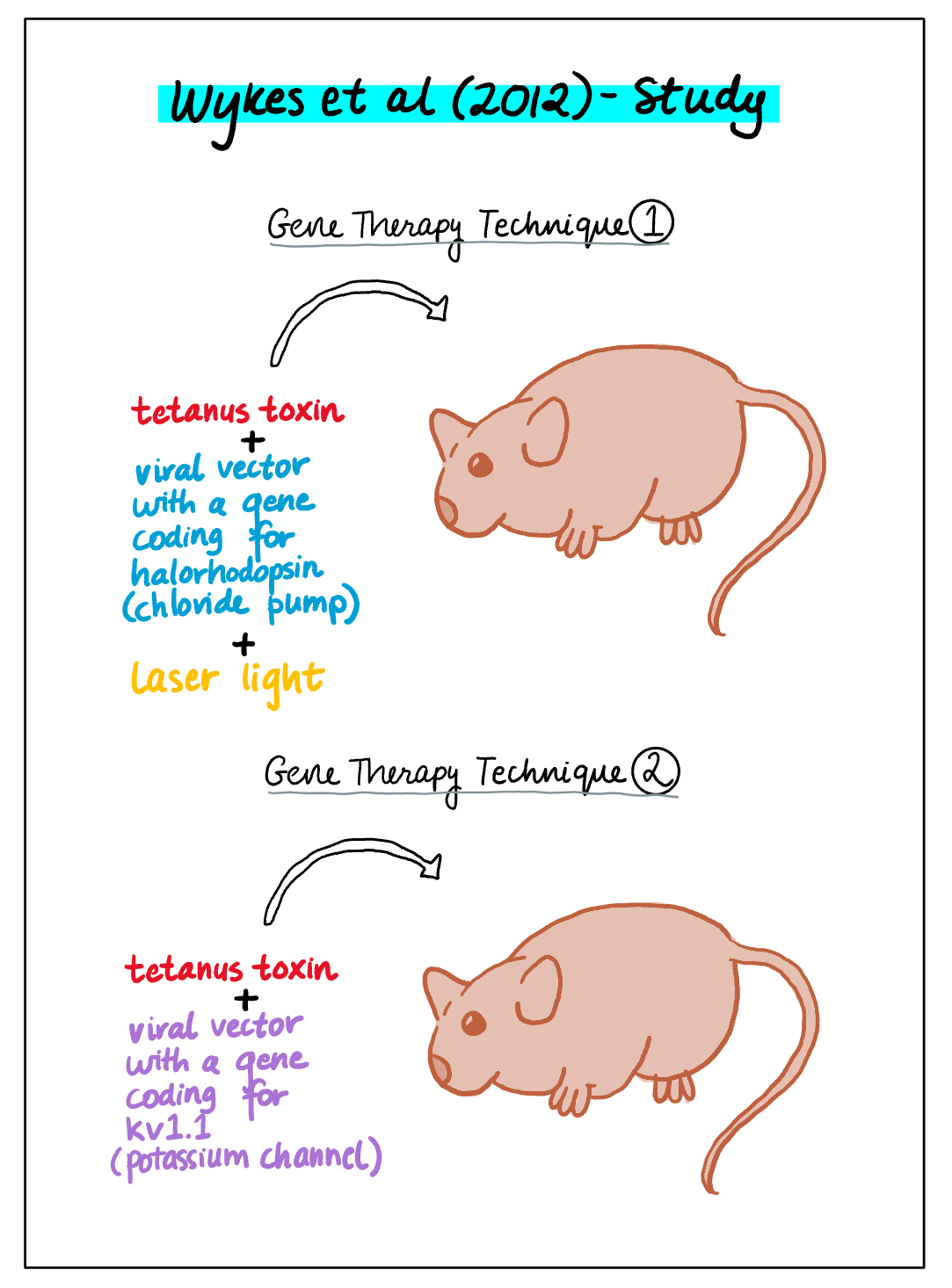
A relatively new area of research being carried out to improve an epilepsy patient’s quality of life is gene therapy, which could be more promising than current methods used by healthcare professionals since it aims to intervene with epileptic tissue at the source. Research by Wykes et al (2012) into gene therapy using rats as subjects has shown findings which could be used to directly target epileptic tissue. In the study, two types of gene therapy techniques were used.
In the first technique, a tetanus toxin was injected into the motor cortex of the rat’s brain which caused the rat to develop focal epilepsy. At the same time, a viral vector was used to transport a particular gene into the rat’s brain - this gene coded for halorhodopsin, a chloride pump or protein that is activated by light. Using an optic fibre, laser light was then delivered into the rat’s brain in order to activate halorhodopsin on the membranes of excitatory neurons - a technique known as optogenetics. As a result of the chloride pumps’ activation, more negative chloride ions were allowed to enter the neurons, causing hyperpolarisation or a more negative charge inside the neurons. This reduced the excitation within the neural networks and therefore lowered epileptic activity, as shown in an EEG test.
In the second technique, a tetanus toxin was once again injected into the rat’s brain, causing focal epilepsy. This time, a viral vector was used to transport a gene into the rat’s brain which coded for a potassium channel known as kv1.1. The overexpression of the inserted gene caused the potassium channels to be used more than normal for transporting positive potassium ions out of the neurons, leading to a more negative charge inside the neurons or hyperpolarisation, reducing epileptic activity. For some rats, the researchers waited until the tetanus toxin had already caused epilepsy and then inserted the viral vector. The EEG test showed that over multiple weeks, epileptic activity not only reduced but also gradually disappeared in these rats. Interestingly, if the viral vector was inserted into the rat’s brain at the same time as the tetanus toxin, the overexpression of the gene completely prevented the rat’s brain from developing epilepsy.
Most current methods for dealing with epilepsy aim to reduce the negative impact of seizures without directly targeting epileptic networks. The findings from Wykes et al (2012) therefore look promising since the gene therapy techniques used by the researchers act at the source of the disorder and aim to permanently reduce the excitability of the seizure-causing networks (see figure 3). However, it is important for multiple clinical trials to be carried out since gene therapies could also have potential risks - for instance, genes that are inserted incorrectly in the DNA could cause tumours. Additionally, viruses are normally used as vectors, so the body could detect these as foreign and therefore cause a severe immune response.
Figure 3: A diagram outlining the two gene therapy techniques utilised by Wykes et al (2012) to treat focal epilepsy in rats.
Since epilepsy is a spectrum disorder, it can have a range of symptoms and outcomes depending on the individual patient. Therefore, it is difficult to isolate a singular method for dealing with the symptoms of epilepsy. While anti-epileptic medication and surgical intervention can help reduce the severity of seizures, they do not work successfully on all patients - Ella is a real-life example whose condition only changed after switching to alternative medicine and going through hormonal changes during puberty. Carrying out further research into methods like alternative medicine and gene therapy could therefore provide promising groundwork for treating epilepsy more successfully in the future - across a wider range of patients.